Introduction
Claim denials represent some of the largest revenue losses for healthcare practices. According to research, an estimated 15-20% of all medical claims have an initial denial, and almost 60% of these claims will never be resubmitted, resulting in a permanent loss of revenue. Effective denial management is necessary for healthcare practices.
It requires proper documentation, coding practices, smooth verification, and other important strategies. This blog outlines the top 7 proven strategies to reduce claim denials and strengthen your revenue cycle.
Verify Patient Eligibility and Benefits in Real-Time
Verification of the patient’s eligibility and benefits before delivering any healthcare services is necessary to prevent denials. Eligibility issues are the most significant preventable source of claim denials and account for approximately 25% of all healthcare practice denials.
In order to limit this issue, providers need to verify patient coverage prior to delivering any services. For verifying eligibility for patients, this process should include: verifying the patient’s active insurance, reviewing the plan-specific coverage limitations, validating copayments, deductibles, prior authorizations, and checking for any exclusions that may impact how much they will be reimbursed by their respective health plan.
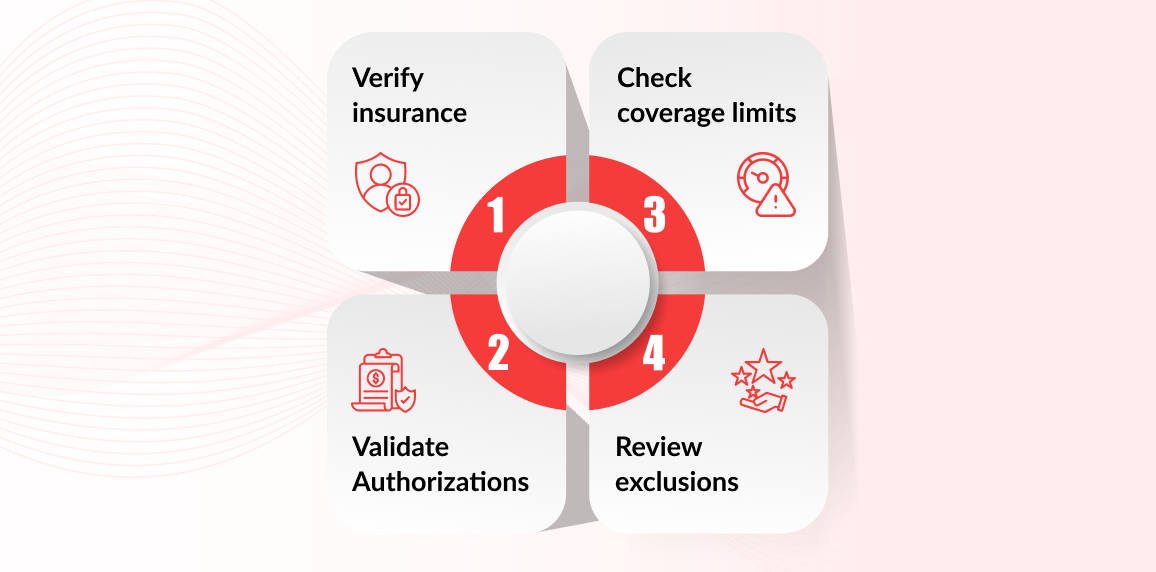
Performing real-time patient eligibility verification enables the practice to receive accurate financial and insurance coverage information upfront, thus eliminating unnecessary claim rejections and delays in payment.
Keep Patient Data Accurate and Complete
Entering incorrect simple demographic information can cost practices thousands of dollars per year. Accurate patient data is necessary to prevent claim denials. It is preferable to verify all entries in regards to patients' names, DOB, insurance IDs, mailing addresses, and referring doctors before submitting claims.

Claim denials can be managed properly by putting the correct first, last names, and digits. Doing this will simplify payment. For reducing claims denials, use the Electronic Health Record EHR's automatic alerts that can indicate incomplete or inconsistent fields prior to submitting your claim, ensuring each claim is correct and complete before submission.
Improve Documentation and Coding Accuracy
Coding-related denials are one of the most preventable causes of lost revenue in medical billing. While code matching, the use of the correct ICD-10, CPT, HCPCS, and modifiers is critical for the prevention of claim denials. Claims denial can be minimized through documenting the medical necessity of the procedure, keeping codes current for newly added procedures, and avoiding upcoding or undercoding.
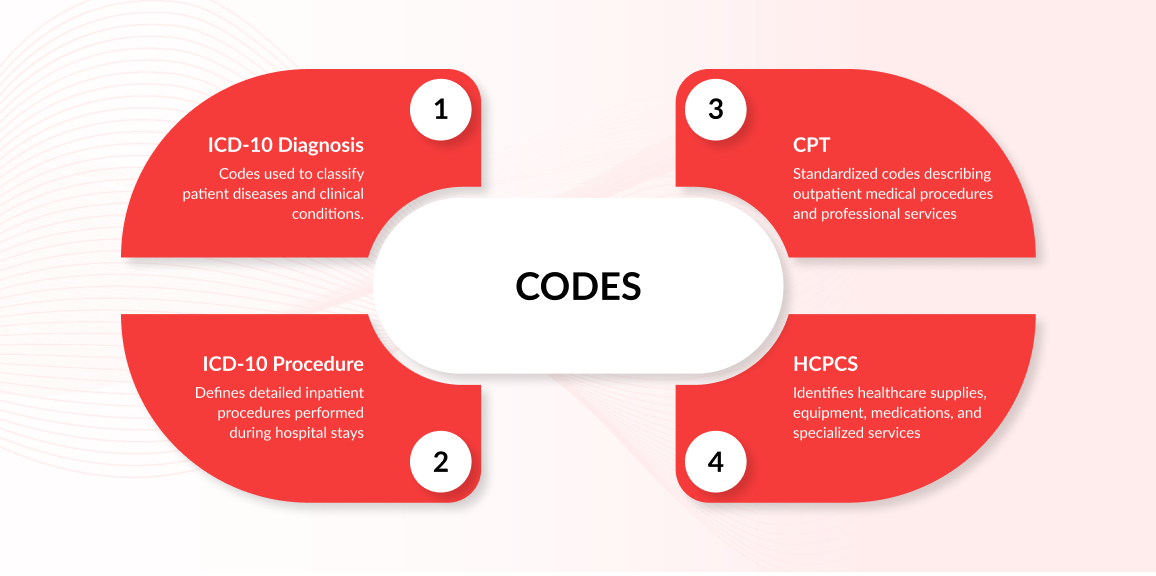
Coding accurately, with proper documentation, will help reduce the number of claim rejections and expedite your ability to receive payment, leading to improved denial management process in medical billing.
The following table shows common code errors, impacts of wrong coding on medical billing, and the preventive measures as well:
Common Coding Errors & Prevention
| Common Issue | Impact | Prevention |
|---|---|---|
| Incorrect modifier | Service considered invalid | Use CMS modifier guidelines |
| Missing diagnosis linkage | Claim rejected for “medical necessity” | Cross-check ICD-10–CPT mapping |
| Outdated codes | Claim automatically denied | Regular coding audits |
Implement Pre-Authorization Workflows
Missing pre-approval authorization is also a contributory factor (almost 12–15%) in medical billing denials. Implementing pre-authorization workflows can help reduce claims denial by simplifying and streamlining billing. To prepare for pre-authorizations, create standard operating procedures for pre-authorization requests, and set up a process for keeping track of authorization numbers. Utilize automated notification systems to alert you when documentation is missing, to prevent claim submissions.
An example of medical services that require pre-authorizations is MRIs and CT scans; claims for these services will be denied immediately—even if the service is deemed medically necessary—if pre-authorization has not been obtained ahead of time. By establishing workflows for pre-authorizations, the medical practice can improve its revenue cycle and eliminate delays.
Conduct Regular Denial Trend Analysis
One of the key components of denial management is exploring and analyzing the reasons, impacts of claim denial. Identifying trends on the highest denial codes by payor, the types of denials seen in the hospitals' departments, and the average turnaround time for appeals will help to reveal the systemic issues.
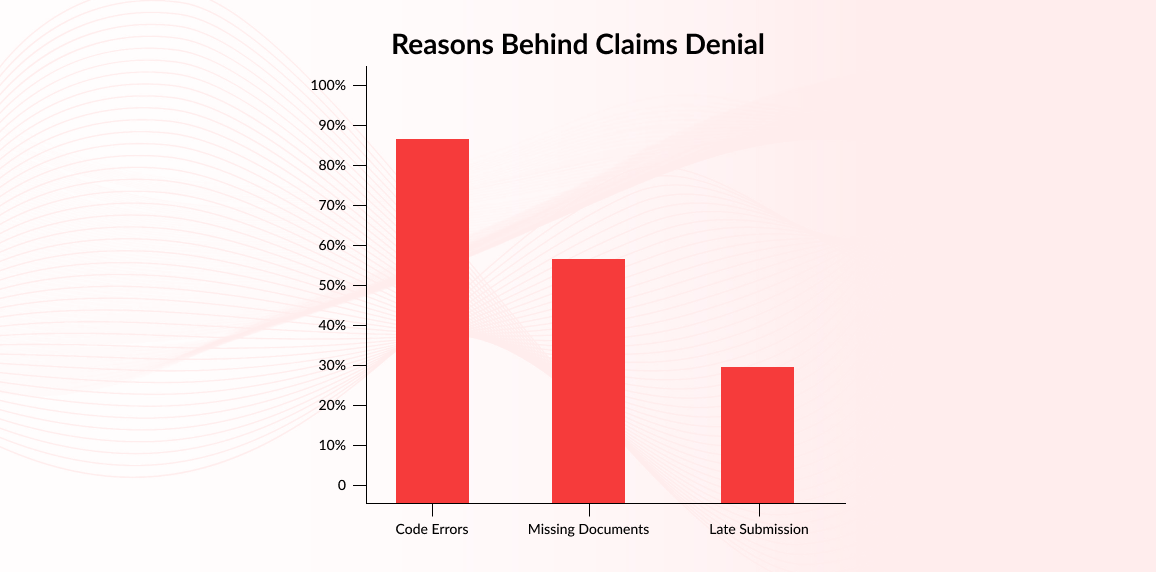
From these insights, targeted corrective actions can be developed to eliminate the root causes of future denials, streamline workflows, and optimize the revenue cycle. For example, if a payor tends to deny claims based on missing documentation, error mismatch, or any other factor, creating a dedicated checklist for that particular payor can significantly reduce the number of denials.
Strengthen Staff Training and SOPs
The number of claim denials is also increased by poor staff training. Consistent and uninterrupted staff training is coupled with appropriate Standard Operating Procedures (SOPs) that have been continuously documented, permitting personnel to work faster and more consistently, resulting in decreased denials, better performance of your team and improved revenue cycle by reducing inconsistencies and minimizing avoidable errors.
1. Building Coding Accuracy Through Training
As staff members participate in regular training, they will be exposed to new codes that were added to CPT, ICD-10, and HCPCS as well as changes to payer rules that have occurred more frequently. Consequently, staff members will have the ability to code a claim accurately without the need to go back and fix it. When you are in compliance with payer coding requirements and can correctly code claims, it will reduce the number of claims denied for coding errors, support compliance, and create accurate representations of your patient's clinical condition.
2. Standardizing Documentation and Charge Capture
It is important that every team member document patient encounters and enter charges in the same manner. By having SOPs in place for the preparation of documentation, charge entry, and claims submission, your team will minimize variability in the way documentation is entered and the way charges are submitted. By having SOPs, your team will create a consistent, structured way to document and enter charges, thus helping them to be better prepared for audits and improving the accuracy of what is being documented and billed.
3. Enhancing Workflow Efficiency
With clearly defined workflows, employees spend less time trying to fix their mistakes and, as a result, are able to complete their duties in a shorter amount of time. By having clearly defined roles and employing streamlined processes, teams can efficiently and consistently evolve claims through the entire claim process with fewer delays.
Adopt Automated Denial Prevention & Follow-Up Tools
Automated denial prevention and follow-up tools allow for faster and more accurate follow-up, thereby reducing the incidence of manual errors and speeding up claim follow-up. For example, complex revenue cycle management (RCM) systems can identify missing or incorrect data before final submission. It automatically assesses claims compliance to payer guidelines, tracks, and manages denials within minutes of submission. It then automatically generates dashboards that show denial trends. With the help of automated RCM processes, you can experience a reduction in claims denials by 20-35% on average.
For instance, an AI-based claim scrubber could detect any discrepancies between an ICD-10 code and corresponding CPT code, preventing a claim from being denied due to lack of medical necessity and allowing for quicker payments. Automating denial management in the medical billing process enables medical billing companies to increase their accuracy and improve efficiency in capturing revenue.
How Denial Prevention Impacts Your Financials
Having a strong denial prevention strategy not only helps reduce claims denial but also provides a safeguard for your practice's financial viability. Every denied claim increases administrative burden and decreases cash flow due to delays in payment.
By eliminating the root cause of denials, healthcare businesses can enjoy better cash flow, faster revenue cycles, and less claim complexities. When claim submissions are clean on the first attempt, practices have an automated payment process that creates quicker payments, fewer charge-offs, and better long-term budgeting.
Conclusion
As previously indicated, reducing claim denials requires a proactive and strategic method to be successful. Utilizing tight eligibility verifications, enhanced documentation, accurate coding practices, and technology will enable medical practices to provide a positive cash flow and minimize lost revenue due to denied claims. A third-party professional medical billing service eliminates these concerns by ensuring claims are properly submitted, processed quickly, and collected in a timely fashion.
If you are looking for dedicated services to reduce claims, Onfinio offers the perfect set of strategies for denial management. Get started with Onfinio’s denial management services and reduce claim denials and revenue loss.
Explore Onfinio’s billing solutions: